By Clarissa Donnelly-DeRoven
Back in August, Lucy Plyler was mailed a 19-page letter from the state health department.
The letter said that the way Victoria, her 24-year-old daughter with multiple disabilities, received Medicaid was about to change. Instead of being in NC Medicaid Direct, Victoria would be put on a “tailored plan.” That meant all her care would no longer be coordinated through the state Department of Health and Human Services, but through the regional behavioral health organization, called an LME-MCO.
Where Plyler and her daughter live in Rutherford County, their LME-MCO would be Partners Health Management.
This switch is happening for nearly 200,000 people out of a total of more than 2.8 million North Carolina Medicaid beneficiaries. These tailored plans are targeted primarily for those with complicated health problems, severe mental health needs, intellectual and developmental disabilities, and traumatic brain injuries. It’s the next phase in the state’s transition to managed care, which started back in July 2021 when about 1.6 million people saw their Medicaid change from being state-run to being coordinated by one of five private insurance companies called managed care organizations.
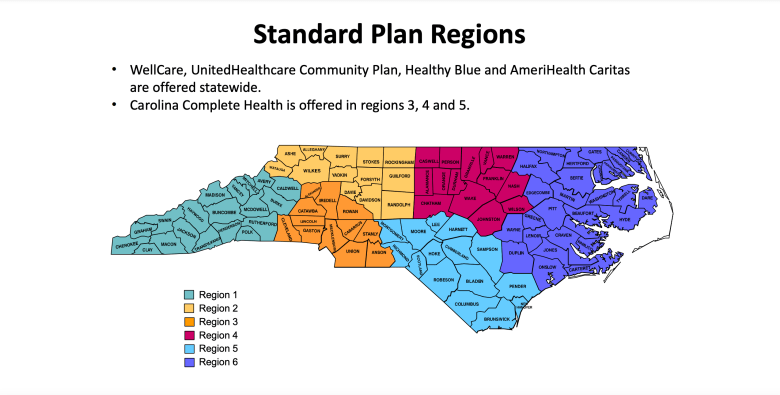 Beginning in July 2021, five managed care companies began administering the majority of the state’s Medicaid program. Four of the programs offer coverage statewide, while Carolina Complete Health offers coverage in a limited region. Credit: North Carolina Department of Health and Human Services
Beginning in July 2021, five managed care companies began administering the majority of the state’s Medicaid program. Four of the programs offer coverage statewide, while Carolina Complete Health offers coverage in a limited region. Credit: North Carolina Department of Health and Human Services
These tailored plans will be quite different from the other managed care plans. Unlike the rest of the Medicaid population, those on tailored plans will not have four to five managed care plans to choose from. In fact, they will have no options to choose from. They will be automatically enrolled in the tailored plan that is run by the LME-MCO that covers their county already.
“The big fear is will a very, very vulnerable population — people with profound disabilities — lose access to care that they really need?” said Doug Sea, an attorney with the Charlotte Center for Legal Advocacy. “The fact is that the General Assembly set this up in a way that directly discriminates against people on the basis of these profound disabilities.
“If you don’t have a disability you can change plans anytime you want, very liberally, and yet these people have no choice of plans.”
For mental health and other providers to keep seeing patients, they have to sign up to be in the LME-MCOs new network. And if they don’t, their patient will have to find a new doctor.
The theory behind this is that the LME-MCOs are more familiar with this population — many people have already been receiving services through them. The idea is that this makes the agencies better equipped than standard managed care plans, which focus on people who have more everyday health needs.
The LME-MCO plans will also include some services, such as medically monitored detox or intensive outpatient substance use treatment, that the standard managed care plans don’t cover.
But, the LME-MCOs have already run into problems building up networks of physical healthcare providers to augment the mental health services they’ve been designed to provide. The state health department cited this on Thursday as the main reason they’re delaying the rollout of tailored plans from Dec. 1 to April 1, 2023.
“We were concerned that we didn’t have the depth of network that we wanted across the state,” said Dave Richard, the deputy secretary for NC Medicaid. By depth of network, he means that there weren’t enough providers enrolled to be “in-network” with the new tailored plans as there needs to be.
“They may have been able to get there,” he said, “but what we didn’t want to do is to launch on December 1, and have the relationships between individuals and their families with their physical health providers disrupted.”
‘A horrible choice’
Some of the tailored plans are subcontracting with one of the five insurance companies that run Medicaid managed care for the rest of the state. Others — Vaya and Alliance — are building up their own networks.
Four of the five managed care organizations cover the entire state. But, two of the LME-MCOs, Partners Behavioral Health Management and Trillium, made the confusing choice to contract with the only managed care organization — Carolina Complete Health — that does not cover the entire state.
In fact, Carolina Complete Health does not currently cover 28 of the counties that Partners and Trillium are supposed to serve.
DHHS published a report last year tallying the number of people in each county who will likely be on tailored plans. In those 28 counties, there are nearly 34,400 people who will qualify for tailored plans, a sizable proportion of the total tailored plan population.
Richard said that all of the plans are required to adhere to federal guidelines set by the Centers for Medicare and Medicaid Services that insure that their networks have enough providers in all the places they have patients.
How they get there is largely up to the LME-MCOs to figure out.
If the tailored plans have built up their provider networks, but many people’s doctors still haven’t joined, the people on these plans could have very limited options.
“For most people, the letter will say ‘You can go back to a standard plan if you want to. You’ve been auto enrolled in a tailored plan, but if you want to go back to the standard plan, you can by giving up these services,’” explained Sea. Many of those services people would have to forfeit are critical to helping people with complex problems function with more ease.
“So, that is a choice,” he said. “It’s just a horrible choice.”
Burden shifts to patients, families
If all this sounds confusing, that’s because it is.
“One of the things that I hear a lot is, ‘Can you explain it simply?’” said Corye Dunn, the director of public policy at Disability Rights.
She said that’s not possible.
“Because it is not simple. There is nothing simple or straightforward about it,” Dunn said.
Asking someone with a profound disability to find a new doctor is also not simple. Often people who need tailored plans have complicated physical conditions tied to their disabilities, and most doctors don’t have the knowledge or experience to treat them.
Victoria, for example, suffers from repeated bouts of skin cancer due to one of her conditions. She and her mother regularly travel to Chapel Hill so she can be treated by a specialist at UNC Hospital. That specialist is not currently in-network with Partners, and if they don’t join, she’ll either need to find a new doctor or pay out of pocket.
“In one of the plans I looked at, I think it was the tailored plan, her doctors were not listed,” said her mom, Lucy. “The LME told me I needed to reach out to my daughter’s doctors and ask them to consider being on the tailored plan.
“I don’t think that’s my job.”
Sea, from the Charlotte Center for Legal Advocacy, argues the burden for building up adequate provider networks should fall on the LME-MCOs, not on patients or their families.
Sign up for our Newsletter
“Another thing that could be done would be to require the LMEs to identify and aggressively reach out to these current providers for this population and go to all lengths necessary to contract, including paying higher rates if need be,” he said.
Getting providers to join these new networks is no small ask. Before July 2021, providers only had to deal with one system for all their Medicaid patients. After the launch of managed care, that increased to six. And with tailored plans, it could be as many as 11 new billing systems — a significant administrative burden.
In most states with Medicaid managed care, states “carve out” most of the really complicated patients – such as people with multiple medical problems, or people with complicated mental health or substance use issues – leaving the insurance companies that run the plans to only cover patients with relatively straightforward health problems.
But North Carolina lawmakers wanted to get all of the state’s Medicaid beneficiaries into managed care. So, DHHS’s proposal has been to create these tailored plans to do that. In addition, North Carolina’s already got a complicated mental health care delivery system.
Many advocates question why the group of people with the highest level of needs will have the fewest options to choose from when it comes to their medical care.
“We have been asking that question since the very beginning,” Dunn said. “We could have had regional and statewide options. We could have allowed more people to stay in Medicaid Direct. There were other options that the state did not choose.
“It’s not all misguided, but it certainly wasn’t a decision that was made primarily about enrollees.”
Republish This Story

Republish our articles for free, online or in print, under a Creative Commons license.


